Page 131 - 《中国药房》2022年14期
P. 131
但该给药方案的安全性还需进一步验证。 Augmented renal clearance in the critically ill:how to
3.5 抗菌药物剂量推荐 assess kidney function[J]. Ann Pharmacother,2012,46(7/
笔者根据近几年的文献及相关综述,对经肾脏排泄 8):952-959.
的常用抗菌药物用于 ARC 患者的给药剂量进行整理, [ 7 ] MAY C C,ARORA S,PARLI S E,et al. Augmented renal
clearance in patients with subarachnoid hemorrhage[J].
结果见表2。
Neurocrit Care,2015,23(3):374-379.
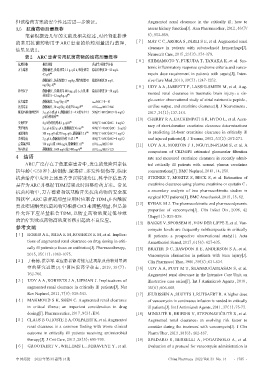
表2 ARC患者常用抗菌药物的给药剂量推荐
[ 8 ] SHIMAMOTO Y,FUKUDA T,TANAKA K,et al. Sys-
抗菌药物 推荐剂量 药动学/药效学目标 temic inflammatory response syndrome criteria and vanco-
万古霉素 静脉滴注,负荷剂量1.5 g、q12 h,维持剂量 稳态谷浓度20~25 mg/L
4.5 g/d [16] mycin dose requirement in patients with sepsis[J]. Inten-
静脉滴注,负荷剂量15 mg/kg,维持剂量42 稳态谷浓度20 mg/L sive Care Med,2013,39(7):1247-1252.
mg/(kg·d) [4] [ 9 ] UDY A A,JARRETT P,LASSIG-SMITH M,et al. Aug-
替考拉宁 静脉滴注,负荷剂量800 mg、q12 h、3剂,维 稳态谷浓度10~30 mg/L mented renal clearance in traumatic brain injury:a sin-
持剂量 8~12 mg/kg、qd [21]
gle-center observational study of atrial natriuretic peptide,
庆大霉素 静脉滴注,7 mg/(kg·d) [23] cmax/MIC≥8~10
达托霉素 静脉滴注,10 mg/(kg·d)或750 mg/d [24] AUC0-24 h/MIC≥666 cardiac output,and creatinine clearance[J]. J Neurotrauma,
哌拉西林/他唑巴坦 3 g、q6 h或q8 h、静脉滴注3~4 h或至少12 50%f T>MIC(MIC=16 mg/L) 2017,34(1):137-144.
g/d持续给药 [30]
[10] CHERRY R A,EACHEMPATI S R,HYDO L,et al. Accu-
头孢匹罗 4 g/d持续给药或1 g、q4 h [35] 60%f T>MIC(MIC=4 mg/L) racy of short-duration creatinine clearance determinations
美罗培南 2 g、q6 h或2 g、q4 h,静脉滴注30 min [38] 60%f T>4 MIC(MIC=2 mg/L)
亚胺培南 500 mg、q4 h或750 mg、q6 h,静脉滴注2 h [39] 90%f T>MIC(MIC=1 mg/L) in predicting 24-hour creatinine clearance in critically ill
多利培南 2 g、q8 h,静脉滴注持续1 h以上 [40] 40%f T>MIC(MIC=8 mg/L) and injured patients[J]. J Trauma,2002,53(2):267-271.
左氧氟沙星 750 mg/d或1 000 mg/d,静脉滴注1 h [41] AUC0-24 h/MIC≥80 [11] UDY A A,MORTON F J,NGUYEN-PHAM S,et al. A
环丙沙星 静脉滴注,1 600 mg/d或2 400 mg/d [42] AUC0-24 h/MIC≥125
comparison of CKD-EPI estimated glomerular filtration
4 结语 rate and measured creatinine clearance in recently admit-
ARC广泛存在于危重症患者中,发生的危险因素包 ted critically ill patients with normal plasma creatinine
括年龄(≤50 岁)、脑创伤、脓毒症、多发性创伤等,临床 concentrations[J]. BMC Nephrol,2013,14:250.
抗菌治疗中应对上述患者予以特别关注,科学评估患者 [12] STEINKE T,MORITZ S,BECK S,et al. Estimation of
是否为ARC并根据TDM结果及时调整给药方案。常见 creatinine clearance using plasma creatinine or cystatin C:
抗菌药物中,万古霉素和氨基糖苷类抗菌药物的安全范 a secondary analysis of two pharmacokinetic studies in
surgical ICU patients[J]. BMC Anesthesiol,2015,15:62.
围狭窄,ARC患者超剂量应用时应联合TDM;β-内酰胺
[13] RYBAK M J. The pharmacokinetic and pharmacodynamic
类及喹诺酮类抗菌药物可根据CrCl来调整剂量,但是条
properties of vancomycin[J]. Clin Infect Dis,2006,42
件允许下应尽量联合 TDM,以防止药物浓度过低导致
(Suppl 1):S35-S39.
的治疗失败或药物高浓度蓄积引起的不良反应。
[14] BAKKE V,SPORSEM H,VON DER LIPPE E,et al. Van-
参考文献 comycin levels are frequently subtherapeutic in critically
[ 1 ] HOBBS A L,SHEA K M,ROBERTS K M,et al. Implica- ill patients:a prospective observational study[J]. Acta
tions of augmented renal clearance on drug dosing in criti- Anaesthesiol Scand,2017,61(6):627-635.
cally ill patients:a focus on antibiotics[J]. Pharmacotherapy, [15] BRATER D C,BAWDON R E,ANDERSON S A,et al.
2015,35(11):1063-1075. Vancomycin elimination in patients with burn injury[J].
[ 2 ] 丁楠楠,洪学军.重症患者肾功能亢进现象及药物剂量调 Clin Pharmacol Ther,1986,39(6):631-634.
整的研究进展[J].中国医院药学杂志,2019,39(7): [16] UDY A A,PUTT M T,SHANMUGATHASAN S,et al.
762-766. Augmented renal clearance in the Intensive Care Unit:an
[ 3 ] UDY A A,ROBERTS J A,LIPMAN J. Implications of illustrative case series[J]. Int J Antimicrob Agents,2010,
augmented renal clearance in critically ill patients[J]. Nat 35(6):606-608.
Rev Nephrol,2011,7(9):539-543. [17] JEURISSEN A,SLUYTS I,RUTSAERT R. A higher dose
[ 4 ] MAHMOUD S H,SHEN C. Augmented renal clearance of vancomycin in continuous infusion is needed in critically
in critical illness:an important consideration in drug ill patients[J]. Int J Antimicrob Agents,2011,37(1):75-77.
dosing[J]. Pharmaceutics,2017,9(3):E36. [18] MINKUTĖ R,BRIEDIS V,STEPONAVIČIŪTĖ R,et al.
[ 5 ] CLAUS B O,HOSTE E A,COLPAERT K,et al. Augmented Augmented renal clearance:an evolving risk factor to
renal clearance is a common finding with worse clinical consider during the treatment with vancomycin[J]. J Clin
outcome in critically ill patients receiving antimicrobial Pharm Ther,2013,38(6):462-467.
therapy[J]. J Crit Care,2013,28(5):695-700. [19] SPADARO S,BERSELLI A,FOGAGNOLO A,et al.
[ 6 ] GROOTAERT V,WILLEMS L,DEBAVEYE Y,et al. Evaluation of a protocol for vancomycin administration in
中国药房 2022年第33卷第14期 China Pharmacy 2022 Vol. 33 No. 14 ·1785 ·